In the fast-paced world of medical technology, healthcare device testing and validation play a critical role in ensuring that products meet stringent regulatory requirements and deliver reliable outcomes. These processes safeguard patient safety, optimize device performance, and build trust among healthcare providers and patients. This article dives into the nuances of healthcare device testing and validation, offering insights from the perspective of an expert in medical and wellness devices.
Table of Contents
Why Healthcare Device Testing and Validation Are Critical
Ensuring Patient Safety
At the heart of any medical device development process lies patient safety. Healthcare devices, from diagnostic tools to life-support systems, directly impact human lives. Rigorous testing ensures that devices function correctly under various conditions and do not pose unforeseen risks to users.
Regulatory Compliance
Meeting global regulatory standards, such as those set by the FDA in the U.S. or CE marking in Europe, is mandatory for market entry. Testing and validation ensure that devices comply with these regulations, streamlining the approval process.
Product Reliability and Reputation
Reliable devices not only enhance patient outcomes but also protect the manufacturer’s reputation. A validated device minimizes risks of recalls or lawsuits, contributing to long-term market success.
Key Phases of Healthcare Device Testing and Validation
1. Concept and Feasibility Testing
This phase involves verifying the basic functionality of the device concept. Developers must assess technical feasibility, identify risks, and gather preliminary data on performance.
Example Tests:
- Prototyping and initial performance checks.
- Compatibility with intended use cases.
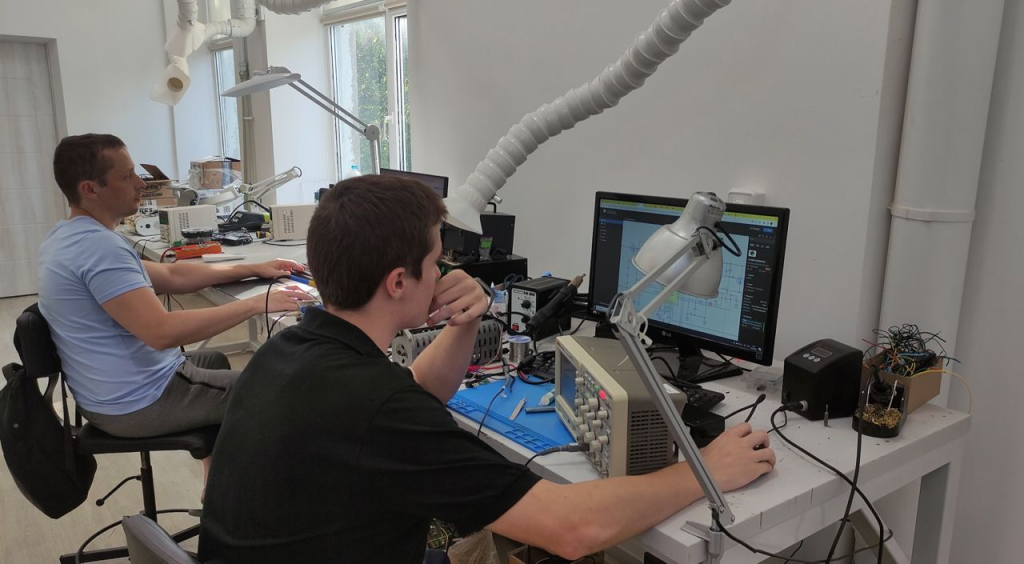
2. Design Verification
During this phase, the device design is tested against the specifications outlined in the design input. Verification confirms that the device performs as intended.
Methods:
- Bench testing using simulated conditions.
- Electrical, mechanical, and software testing.
- Ensuring alignment with regulatory standards.
3. Design Validation
Unlike verification, which focuses on meeting design specifications, validation ensures the device meets user needs and performs effectively in real-world conditions.
Example Processes:
- Usability testing with end-users.
- Clinical trials or simulated clinical environments.
4. Preclinical Testing
Preclinical testing evaluates the biological and mechanical compatibility of devices. This step is especially crucial for implantable devices.
Typical Tests:
- Biocompatibility testing (ISO 10993).
- Sterility and packaging integrity tests.
- Accelerated aging studies.
5. Clinical Validation
Involving human participants, clinical validation focuses on the safety and efficacy of the device in its intended environment. These trials are often required for regulatory submissions.
6. Production Validation and Quality Control
Once a device is ready for manufacturing, production validation ensures that the manufacturing process consistently produces devices that meet specifications. Quality control measures are implemented to maintain these standards.
Tools:
- Process validation techniques.
- Statistical quality control (SQC).
Common Challenges in Healthcare Device Testing and Validation
Regulatory Complexity
Navigating the intricate web of regional and international regulations can be daunting. Each market may have unique requirements that must be addressed.
Accelerated Timelines
Startups and large corporations alike face pressure to reduce time-to-market. While speed is essential, it should not compromise testing thoroughness.
Resource Constraints
Testing and validation demand specialized expertise, equipment, and significant financial investment.
Best Practices for Effective Testing and Validation
- Start Early: Incorporate testing at the earliest stages of development to identify potential issues.
- Use Realistic Simulations: Testing under real-world conditions offers more reliable data.
- Engage Stakeholders: Involve clinicians, patients, and regulatory experts throughout the process.
- Adopt Automation: Automated testing tools can streamline processes and improve accuracy.
- Iterate and Optimize: Use feedback from each testing phase to refine the device design.

Emerging Trends in Healthcare Device Testing and Validation
Artificial Intelligence (AI) Integration
AI-driven tools are revolutionizing testing by predicting device performance and identifying potential failures more efficiently.
Digital Twins
Digital twins allow developers to create virtual replicas of devices for testing in simulated environments, saving time and costs.
Focus on Cybersecurity
As devices become increasingly connected, cybersecurity validation is paramount to protect patient data and device functionality.
Conclusion
Healthcare device testing and validation are indispensable for ensuring reliable outcomes and safeguarding patient safety. By adopting a structured, phased approach and leveraging modern tools and technologies, developers can streamline these processes, meet regulatory requirements, and bring effective devices to market with confidence.
For more insights into medical device development, check out my detailed guide on Medical Device Engineering.
What challenges have you encountered in the testing and validation process for healthcare devices, and how have you addressed them? Let’s start a conversation!



 430 Park Ave, New York, NY 10022, USA
430 Park Ave, New York, NY 10022, USA Paevalille tn 6, Office 84, Estonia, Tallinn, 13517
Paevalille tn 6, Office 84, Estonia, Tallinn, 13517 Barykadna St 7, Dnipro, Ukraine, 49000
Barykadna St 7, Dnipro, Ukraine, 49000